Unique device. German scientists have developed a new method of multispectral optical-acoustic tomography
The device was created by physicists of the International Scientific and Educational Laser Center of Moscow State University. M.V. Lomonosov on the basis of two long-known phenomena. First, a cancerous tumor absorbs light and heat more intensely than healthy tissue, which has a lower concentration of blood and more oxygen.
In addition, it is known that all bodies, when heated, not only expand, but also emit a sound. Consider, for example, how a boiling kettle whistles. Moreover, slow heating generates a weak sound. Fast is more powerful. And the instant gives a powerful acoustic wave.
So, the "singing tomograph" almost instantly heats the tissue under study with its laser beam: in a hundredth of a microsecond - by one tenth of a degree. Since there is more blood in any tumor than in healthy tissues, it heats up more. And the sound coming from it is two to three times more powerful. It is captured by the ultra-sensitive acoustic system of the tomograph. This "electronic ear" pinpoints the exact location of the tumor.
The sound signal on the computer screen turns into a picture. A bright yellow spot in a blood-red frame on a black background looks like a cosmic landscape. You can even admire them if you don’t know that this is a snapshot of a cancerous tumor. It is hundreds of times more contrast than any image of her made by already known methods.
This general principle operation of the device, - explains the project manager, Doctor of Physical and Mathematical Sciences Alexander Karabutov. - In reality, tomography takes place in two steps. First, a laser beam of a certain wavelength scans the patient's chest. So far, this is just a search for inhomogeneities. If the tomograph "hears" a sharp increase in sound, then a suspicious place has been found. But what is it? Malignant or benign education? We switch the device to another wave, which checks the blood in the found tumor for the level of oxygen content. If it is less than normal, it is cancer. What the tomograph reports. He "sings" again, but "not in his own voice": the timbre changes significantly. But if the oxygen concentration is above the norm, then the timbre of the sound is completely different. This is most likely just mastopathy.
An ordinary laboratory assistant can process acoustic signals. And after a few minutes, get on the computer screen an image of a tumor - if, of course, there is one - ranging in size from 2 millimeters at a depth of up to 7 centimeters. And also to find out whether it is benign or not. All this without any harm to the patient. And painless. It is in these "four in one" that the uniqueness of the "singing tomograph" lies.
For comparison, the same x-ray or neutron capture diagnostic technologies, like any radioactive exposure, are not harmless even for a healthy person. And modern means, for example, optical diagnostics, make it possible to determine a tumor of at least five millimeters. Moreover, breast cancer, which does not yet metastasize, is only three millimeters. It is all the more difficult to distinguish such a "grain" by optical method if it lies at a depth of, for example, six centimeters. After all, the beam must pass through the entire female breast - back and forth. And this is the medium that scatters light. On the way there, it scatters a million times, back - also a million. But the sound does not undergo any serious distortion. Therefore, an optical signal converted into an acoustic one gives a much higher diagnostic accuracy.
Just awarded Nobel Prize nuclear magnetic tomography, with absolute harmlessness, gives a three-dimensional image of a tumor lying at any depth. But it also has a very significant drawback: what is good for brain research falters with mammography. The study on NMT lasts twenty minutes: the patient breathes, the blood pulsates, both its concentration and the level of oxygen content change. The picture is obtained with significant distortion. It happens that a nuclear magnetic tomogram is diagnosed as cancer, but then a biopsy gives a negative conclusion.
Yes, we get only a two-dimensional image, - says Alexander Karabutov, - but practically without distortion. Indeed, in a third of a second, too strong physiological changes in the tissue under study do not occur. Our tomograph does not replace all known ones, it complements them.
While the "singing tomograph" exists only in laboratory version. And yet, two dozen volunteers with suspected malignant tumors have already been examined on it. The instrument has never made a mistake. And one of the women came up with such a story. The fact that she had cancer was indicated by various tests. But where he is hiding, could not be revealed by any known means. It turned out to be behind a silicone implant. This was reported by the laser optoacoustic tomograph.
Laser tomography as a method of diagnosing diseases
Tomography (Greek tomos layer, piece + graphiō to write, depict) is a method of non-destructive layer-by-layer study of the internal structure of an object by means of its repeated transillumination in various intersecting directions (the so-called scanning transillumination).
γ-quantum511 keV |
tomography |
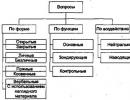
Types of tomography
Today, organs inside the body are diagnosed mainly by X-ray (CT), magnetic resonance (MRI) and ultrasound (UST) methods. These methods have high spatial resolution, providing accurate structural information. However, they have one common drawback: they cannot determine whether a particular spot is a tumor, and if so, then is it malignant. In addition, X-ray tomography cannot be used before 30 years.
MULTIMODALITY! Consistent use of different methods - one with good spatial resolution
Cathode Beam CT - 5th generation
Anterior CT (left), PET (center), and Combined PET/CT
(right), showing the distribution of positrons emitted by 18 F-fluorodioxide glucose superimposed on CT

Laser Optical Tomography
Optical, and primarily interference measurements, have made a significant contribution to the development of physical and instrumental optics, as well as to the improvement of measurement technology and metrology. These measurements have an exceptionally high accuracy over a wide range of measured values, due to the use of light wavelength as a measure and technically simply reproducible in laboratory and production conditions. The use of lasers not only provided new functional and metrological possibilities of optical interferometry, but also led to the development of fundamentally new methods of interference measurements, such as interferometry using low-herence optical radiation, which ensures the formation of an interference signal only at small differences in the wave paths in the interferometer.
Low-coherence interference systems operate in the mode of the so-called correlation radar, which determines the distance to the target by the position of the correlation pulse signal, which is the interference signal in the interferometer. The shorter the coherence (correlation) length, the shorter the duration of the correlation pulse and the more accurately the distance to the target is determined, in other words, the higher the spatial resolution of the radar. Achievable values of the coherence length of optical radiation in units of micrometers, respectively, provide micron resolution of the optical radar. Optical interference radars have found especially wide practical application in biomedical diagnostic equipment (optical tomographs) for monitoring the parameters of the internal structure of biological tissue.
Fluorescent optical tomography is one variation of this idea. The light reflected from the tumor (Fig. 1.11a) differs from the light reflected from normal tissue, and the luminescent characteristics also differ (Fig. 1.11b) due to differences in the degree of oxygenation. To reduce false-negative diagnoses, an IR laser irradiates the tumor through a probe, and then the radiation reflected from the tumor is recorded.

Opto-acoustic tomography uses the difference in the absorption of short laser pulses by tissues, their subsequent heating and extremely rapid thermal expansion, to obtain ultrasonic waves detected by piezoelectrics. It is useful, first of all, in the study of blood perfusion.
Confocal scanning laser tomography (SLO) - used to obtain non-invasive three-dimensional images of the posterior segment of the eye (optic disc and surrounding retinal surface). The laser beam is focused at a certain depth inside the eye, and scanned in a two-dimensional plane. receiver
light reaches only from this focal plane. Subsequence |
|
such flat 2D pictures obtained by increasing the depth of the focal |
|
plane, resulting in a 3D topographic image of the disc |
|
optic nerve and parapapillary retinal layer of nerve |
|
fibers (comparable to standard fundus stereophotography) |
|
Fig.1.10. This approach is useful not only for direct |
|
anomaly detection, but also to track minor |
|
temporary changes. Less than 2 sec required to make |
|
consecutively 64 sweeps (frames) of the retina on the field 15°x15°, |
|
reflected from different depths of the 670-nm laser radiation. Edge shape |
|
fossa underlined by a curved green line indicates a defect |
|
layer of nerve fibers on the framing (rim) of the optic disc. |
Fig.1.10 Confocal scanning laser |
tomography of the optic disc |
confocal microscope
Axial Resolution LimitsSLO |
|||||||
Longitudinal Resolution |
Slo and, |
||||||
respectively, |
confocal z |
||||||
microscope depends on |
|||||||
sharpness is inversely proportional to the square of the numerical aperture (NA=d/2f) of the microobjective. Since the thickness of the eyeball, which takes on the role of a microscope lens, is ~2 cm for a non-dilated pupil NA <0,1. Таким образом,
retinal image depth of field for laser-scanning confocal ophthalmoscopy is limited to >0.3 mm due to the combined effect of low numerical aperture and anterior chamber aberrations.

Optical coherence tomography (OST)
OST, a new medical diagnostic developed in 1991, is attractive for biomedical research and the clinic for several reasons. OST allows you to create a real-time image with µm resolution of cellular dynamics, without the need for conventional biopsy and histology, giving an image of tissues, incl. with strong scattering, such as skin, collagen, dentin and enamel, at a depth of up to 1-3 microns.
What scatters in tissue?
penetration of radiation into |
||||||
biotissue depends on both absorption and |
||||||
scattering. Scattering is associated with different |
||||||
refractive indices in different cells and |
||||||
cell cells. |
||||||
Scattering of light on tissue structures |
||||||
Scattering depends on the wavelength |
||||||
Scattering in tissue occurs at the lipid-water interface in cell membranes (especially |
||||||
laser beam |
(Rice.). Radiation with length |
mitochondrial membranes (a)), nuclei and protein fibers (collagen or actin-myosin (b)) |
||||
waves much larger than the diameter of the cellular structures (>10 µm) are weakly scattered.
Excimer laser radiation in the UV range (193, 248, 308 and 351 µm), as well as IR radiation of 2.9 µm water-induced erbium (Er:YAG) and 10.6 µm CO2 lasers have penetration depths from 1 to 20 µm. Due to the small penetration depth, scattering in the layers of keratinocytes and fibrocytes, as well as on erythrocytes in blood vessels, plays a subordinate role.
For light with a wavelength of 450-590 nm, which corresponds to the lines of argon lasers, KTP / Nd and diode lasers in the visible range, the penetration depth is on average from 0.5 to 3 mm. Like absorption in specific chromophores, scattering plays a significant role here. The laser beam of these wavelengths, although still collimated at the center, is surrounded by a zone of high collateral scattering.
In the spectral region between 590–800 nm and more up to 1320 nm, with relatively weak absorption, scattering also dominates. Most IR diode and well-studied Nd:YAG lasers fall within this spectrum. The penetration depth of radiation is 8-10 mm.
Small tissue structures such as mitochondrial membranes, or the periodicity of collagen fibers, much smaller wavelengths of light (λ), result in isotropic Rayleigh scattering (stronger at shorter wavelengths, ~λ-4 ). Large structures such as whole mitochondria or bundles of collagen fibers, much longer wavelengths of light, lead to anisotropic (forward) Mie scattering (~λ-0.5 ÷ λ-1.5 ).

Optical diagnostics involves the study of biological tissue using ballistic coherent tomography (the time of flight of a photon to the target is detected), or diffuse tomography (the signal is detected after multiple photon scattering). An object hidden within the biological environment must be detected and localized, providing both structural and optical information, preferably in real time and without changing the environment.
Diffuse optical tomography (DOT).
In a typical DOT, tissue is probed with near infrared light transmitted through a multimode fiber applied to the surface of the tissue. Light scattered by tissue is collected from various locations by fibers connected to optical detectors, similar to CT or MRI. But practical
the use of DOT is limited by the strong absorption and scattering of light by the tissue, which results in low resolution compared to standard clinical techniques, X-ray and MRI.
Laser detection of an object in a scattering medium, incl. ommethod of average photon trajectories (PAT).
In addition, the sensitivity of the method decreases with increasing depth, leading to its non-linear dependence across the image area, making it even more difficult to restore large volumes of tissue. tumor vasculature increases its concentration relative to normal tissue) is critical for clinical use.

Principle of Ballistic Coherence Tomography (BCT)
The beam scattered by the object in the Michelson interferometer (the mirror in the object arm of the interferometer is replaced by a biological tissue) interferes with the reference one (the reference arm has a precisely movable retromirror). By changing the delay between the beams, one can obtain interference with a signal from different depths. The delay is continuously scanned, due to which the frequency of light in one of the beams (reference) is shifted due to the Doppler effect. This allows you to highlight the interference signal against a strong background due to scattering. A pair of computer-controlled mirrors, scanning the beam over the surface of the sample, builds a tomographic image processed in real time.
Block diagram and principle of operation of the OST
Spatial depth resolution is determined by the temporal coherence of the light source: below
coherence, less than the minimum thickness of the slice of the image of the object under study. With multiple scattering, optical radiation loses coherence, so you can use
broadband, low-herence, incl. femtosecond lasers for the study of relatively transparent media.True, in this case, too, strong light scattering in biological tissues does not allow one to obtain an image from a depth>2-3 mm.

Axial resolution limitations
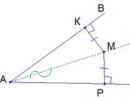
For Gaussian beams d is the size of the beam on the focusing lens with focal length f
OCT axial resolution ∆z as a function of laser radiation spectrum width ∆λ and central wavelength λ
(Assumptions: Gaussian spectrum, non-dispersive medium)
Depth of field
b - confocal parameter = double Rayleigh length
In contrast to confocal microscopy, OCT achieves very high longitudinal image resolution regardless of focusing conditions, as longitudinal and transverse resolution are determined independently.
The lateral resolution as well as the depth of field depend on the size of the focal spot.
(as in microscopy), while longitudinal
resolution depends mainly on the coherence length of the light source ∆z = IC /2 (and
not from the depth of field, as in microscopy).
The coherence length is the spatial width of the autocorrelation field measured by the interferometer. The correlation field envelope is equivalent to the Fourier transform of the power spectral density. Therefore, the longitudinal
resolution is inversely proportional to the spectral bandwidth of the light source
For a central wavelength of 800 nm and a beam diameter of 2-3 mm, neglecting the chromatic aberration of the eye, the depth of field is ~450 µm, which is comparable to the depth of retinal imaging. However, the low numerical aperture NA of the focusing optics (NA=0.1÷0.07) is the low longitudinal resolution of a conventional microscope. The largest pupil size, for which a diffraction resolution of ~3 mm is still preserved, gives a retinal spot size of 10–15 µm.
Reducing spots on the retina, and, accordingly,
increase in transverse resolution of OCT by an order of magnitude, can be achieved by correcting eye aberrations using adaptive optics

OCT axial resolution limitations
Distortion of the shape of an ultra-wide band of the spectrum of a light source
Chromatic aberration of optics
Group velocity dispersion
Chromatic aberration of optics
Achromatic lens (670-1020nm 1:1, DL)
Chromatic aberrations as a function of interferometer focus length for regular and parabolic reflex lenses
Group velocity dispersion
Group velocity dispersion reduces resolution
OST (left) by more than an order of magnitude (right).
Group velocity dispersion correction COST of the retina Thickness of fused silica or BK7 in the reference
leverage varies to compensate for dispersion

(a) Ti:sapphire laser and SLD spectrum width (dotted line)
(b) CMP axial resolution
High resolution optical coherence tomograph
IN unlike X-ray (CT) or MRI tomography, OCT can be designed into a compact, portable
And relatively inexpensive device. Standard resolution OCT(~5-7 µm), determined by the generation bandwidth, is ten times better than that of CT or MRI; ultrasound resolution at optimal transducer frequency ~10
MHz ≈150 µm, at 50 MHz ~30 µm. Main disadvantage OST - limited penetration into opaque biological tissue. The maximum image depth in most tissues (except the eyes!) ~1-2 mm is limited by optical absorption and scattering. This depth of OCT imaging is superficial compared to other techniques; however, it is sufficient to work on the retina. It is comparable to a biopsy and therefore sufficient to assess most of the early changes in neoplasms, which very often occur in the most surface layers, for example, in the epidermis of human skin, mucosa or submucosa of internal organs.
In OCT, in comparison with the classical scheme of an interference microscope, sources with higher power and better spatial coherence (usually superluminescent diodes) and objectives with a small numerical aperture (NA<0,15), что обеспечивает большую глубину фокусировки, в пределах которой селекция слоев осуществляется за счет малой длины когерентности излучения. Поскольку ОСТ основан на волоконной оптике, офтальмологический ОСТ легко встраивается в щелевую лампу биомикроскопа или фундус-камеру, которые передают изображения луча в глаз.
Consider as the central wavelength λ=1 μm (the laser can have Δλ< 0,01нм), и в этом случае l c ≈ 9см. Для сравнения, типичный SLD имеет полосу пропускания Δλ ≥50 нм, т.е. l c <18 мкм и т.к l c определяется для двойного прохода, это приводит к разрешению по глубине 9 мкмв воздухе, которое в тканях, учитывая показатель преломления n ≈1.4, дает 6 мкм. Недорогой компактный широкополосный SLD с центральной длиной волны 890 нм и шириной полосы 150 нм (D-890, Superlum ),
makes it possible to obtain an image of the retina with an axial resolution in air of ~3 μm.
Interference requires a strict relationship between the phases of the interfering waves. With multiple scattering, the phase information disappears, and only singly scattered photons contribute to the interference. Thus, the maximum penetration depth into the COST is determined by the depth of single photon scattering.

Photodetection at the output of the interferometer involves the multiplication of two optical waves, so a weak signal in the object arm, reflected or transmitted through the tissue, is amplified by a strong signal in the reference (reference) arm. This explains the higher sensitivity of OCT compared to confocal microscopy, which, for example, in the skin can only image up to a depth of 0.5 mm.
Since all OCT systems are based on a confocal microscope, the transverse resolution is determined by diffraction. To obtain 3D information, imaging devices are equipped with two orthogonal scanners, one for scanning the object in depth, the other for scanning the object in the transverse direction.
A new generation of OCT is being developed both in the direction of increasing the longitudinal resolution ∆ z= 2ln(2)λ 2 /(π∆λ) ,
by expanding the generation band ∆λ and by increasing |
||
depth of radiation penetration into the tissue. |
||
solid state |
lasers show ultra high |
|
OST permission. Based on broadband Ti:Al2 O3 |
||
laser (λ = 800 nm, τ = 5.4 fsec, bandwidth Δλ up to 350 |
||
nm) was developed with an ultra-high (~1 μm) axial |
||
resolution, an order of magnitude greater than the standard |
||
level of OCT using superluminescent diodes |
||
(SLD). As a result, it was possible to obtain in vivo from the depth |
||
highly scattering tissue image of biological |
||
cells with a spatial resolution close to |
||
diffraction limit of optical microscopy, which |
||
allows for |
tissue biopsy directly into |
The level of development of femtosecond lasers: |
operation time. |
duration<4fs, частота 100 MГц |
|
Since the scattering depends strongly on the wavelength, decreasing with its increase, a greater depth of penetration into the opaque tissue can be achieved with longer wavelength radiation compared to λ=0.8 µm. The optimal wavelengths for obtaining an image of the structure of opaque biological tissues lie in the range of 1.04÷1.5 µm. Today, a broadband Cr:forsterite laser (λ=1250 nm) makes it possible to obtain an OCT image of a cell with an axial resolution of ~6 µm from a depth of up to 2-3 mm. A compact Er fiber laser (supercontinuum 1100-1800 nm) provides a longitudinal OCT resolution of 1.4 µm and a transverse resolution of 3 µm at λ=1375 nm.
Phononic crystal fibers (PCF) with high non-linearity have been used to generate an even wider spectral continuum.
Broadband solid-state lasers and superluminescent diodes cover almost the entire visible and near-IR region of the spectrum, which is most interesting for OCT imaging.
The unique device was designed by physicists from the International Scientific and Educational Laser Center of Moscow State University named after M.V. Lomonosov. It is called a laser optoacoustic tomograph, and it will be used to examine neoplasms in the mammary glands. The device with radiation of one wavelength helps to find inhomogeneity the size of a match head in the patient's chest, and the other - to determine whether this neoplasm is benign or not. With the amazing accuracy of the method, the procedure is completely painless and takes only a few minutes. The authors managed to carry out the work thanks to the support of the Russian Foundation for Basic Research, which highly appreciated this innovative project. Colleagues from the NPP "Antares" helped the scientists to create a prototype of the tomograph.
The instrument is based on two methods. Figuratively speaking, the laser makes the tumor sing, and the acoustic microscope finds and determines its nature by the sound timbre. To implement this principle "in metal", that is, to move from an idea to a prototype, the authors had to develop not only the design of the tomograph, but also the corresponding software. It allows you to obtain an optical image of a tumor hidden at a depth of up to 7 cm and accurately locate its location.
First, a laser comes into play, which can generate radiation at two wavelengths in the near infrared range - of course, sequentially. First, with a beam of one wavelength, the operator scans the patient's chest - while this is a search for tissue inhomogeneities. At the site of irradiation, the tissue heats up a little - literally by a fraction of a degree, and from heating it expands. Since the pulse time is a fraction of a microsecond, this expansion also occurs quickly. And, increasing in volume, the fabric emits a weak acoustic signal - it squeaks softly. Of course, you can only catch the squeak with the help of a highly sensitive receiver and amplifiers. All this is also available in the new tomograph.
Since there are more blood vessels in the tumor, it heats up more than normal tissue, and when heated, it generates an ultrasound signal with different parameters. This means that by "translucent" and "listening" to the chest from all sides, you can find the source of the "wrong" acoustic signal and determine its boundaries.
The next step is the diagnosis of the neoplasm. It is based on the fact that the blood supply of the tumor also differs from the norm: in a malignant tumor, there is less oxygen in the blood than in a benign one. And since the absorption spectra of blood depend on the content of oxygen in it, this makes it possible to determine the nature of the neoplasm. Moreover, it is non-invasive, which means it is painless, fast, and safe. To do this, the researchers proposed using laser infrared radiation with a different wavelength.
As a result, after processing the received acoustic signals, the operator will be able to receive a 5x5 cm image of a 2-3 mm tumor at a depth of up to 7 cm on the device screen in real time and find out whether it is benign or not. “So far, there is only a working layout of the installation,” says Alexander Karabutov, Doctor of Physical and Mathematical Sciences, project manager. “We plan that a prototype of our laser-acoustic tomograph will soon be ready, which we hope to prepare for testing in the clinic by the end of next year. The clinic is waiting for this device."
Read the text and complete tasks A21 - A25. (1)... (2) It is called a laser optoacoustic tomograph, and it will be used to examine neoplasms in the mammary glands. (3) An instrument with one wavelength of radiation helps to find an inhomogeneity the size of a match head in the patient's breast, and another one to determine whether it is a benign neoplasm or not. (4) With the amazing accuracy of the method, the procedure is completely painless and takes only a few minutes, (5) ... the laser makes the tumor sing, and the acoustic microscope finds and determines its nature by the sound timbre. A21. Which of the following sentences should come first in this text? 1) The device is based on two methods at once. 2) The authors managed to carry out the work thanks to the support of the RFBR. 3) The unique device was designed by physicists from the International Scientific and Educational Laser Center of Moscow State University. M. V. Lomonosov. A22. Which of the following words (combinations of words) should be in place of the gap in the fifth (5) sentence? 1) First of all 2) Figuratively speaking 3) In addition A23. What words are the grammatical basis in the fourth (4) sentence of the text? 1) the procedure is completely painless 2) the procedure takes several minutes 3) the procedure takes A24. Indicate the correct description of the fifth (5) sentence of the text. 1) complex, with non-union and allied coordinating connection 2) compound 3) complex non-union А25. Indicate the correct morphological characteristic of the word "this" from the third (3) sentence of the text. 1) personal pronoun 2) demonstrative pronoun 3) definitive pronoun
Similar questions
- Help to understand what is required in the exercise. Correct the sentences and correct. What should be the correct answer... sample.. cows have got short tails. Cows haven "t got short tails. They have got long tails......The bear has a t...
- Are mixtures of two liquids always heterogeneous?
- 1) He put the candle on the table. 2) I got a beautiful present. 3) I am playing the piano now. 4)He has turned off the TV set. 5)We receive e-mails every day. 6)Nick is eating an ice-cream now. 7) She will lend money to...
- how to solve equation a: 1 5/7= 2 2\5: 2 2\35
- What was the name of the estate-representative institution that appeared during the reform period of the Chosen One? 1) Supreme Privy Council 2) Veche 3) Zemsky Sobor 4) State Council